B12 og hypotyreose
➡️ Vitamin B12 er et veldig viktig vitamin og kan forårsake forskjellige symptomer som ligner på hypotyreose.
➡️ Vitamin B12 - mangel kan skyldes pernisiøs anemi, en autoimmun tilstand. Hvis du går til fastlegen din med tretthet som symptom, vil legen sannsynligvis ta en vitamin B12 - test blant flere andre. Det som mange kanskje ikke vet, er at testen som normalt blir tatt er en total B12 - test.
➡️ På samme måte som forholdet mellom totalt T4 og FT4, er totalt B12 bundet til et glykoprotein kalt haptokorrin.
➡️ Imidlertid kan B12 bundet til haptokorrin ikke brukes av de aller fleste cellene i kroppen.
➡️ Bare B12 bundet til transkobalamin (også kjent som holotransobalamin, holoTC eller Aktiv-B12), som er et transportbærerprotein, tas opp fra blodet til cellene i kroppen.
Fire diagnostiske testnøyaktighetsstudier, ved bruk av forskjellige referansestandarder, rapporterte større diagnostisk nøyaktighet for aktiv-B12- analysen sammenlignet med analyser som måler andre markører for vitamin B12-mangel.
Serum holotranscobalamin (holoTC): i serum finnes vitamin B12 i 2 bundne former. Det kan bindes til haptokorrin for å danne holohaptokorrin; eller bundet til transkobalamin for å danne holoTC. Celler kan bare ta opp vitamin B12 i form av holoTC (Hunt et al. 2014). Derfor er måling av holoTC mer reflekterende for vitamin B12 -status enn å måle totalt vitamin B12 eller holohaptokorrin alene. HoloTC kan være en mer pålitelig markør for vitamin B12 -mangel. "

Vitamin B12-mangel hos pasienter med hyptyreose
ABSTRAKT
BAKGRUNN
Hypotyreose er en vanlig endokrin lidelse som rammer 11 % av voksenbefolkningen i vestlige land. Hypotyreose kan forårsake en rekke forskjelligeanemiske lidelser. Pasienter med både hypotyreose og vitamin B12-mangel har også lignende symptomer. Derfor ble denne studien utført for å evaluere forholdet mellom de to og også hypotyreose på grunn av autoimmun årsak.
Department of General Medicine, Rajarajeswari Medical College, Bangalore, Karnataka, India.
👉🏼Pasienter med hypotyreose ble studert for forekomst av mangel på vitamin B12. Det ble funnet at 26 av 50 (52 %) pasienter hadde lave B12-nivåer. Forekomsten hos kvinner (54 %) var høyere enn hos menn (46 %). Vår studie viste sammenheng mellom hypotyreose og vitamin B12-mangel og også autoimmun skjoldbrusksykdom
Pasienter med autoimmun skjoldbruskkjertelsykdom har en høyere forekomst av pernisiøs anemi sammenlignet med den generelle befolkningen.
https://www.b12-foreningen.no/l/n33/
B12-mangel og hypotyreose.
Vitamin B12-mangel er jo som vi vet navnet på en medisinsk tilstand som skyldes for lite av vitaminet B12 i blodet. Hypothyreose er også en mangeltilstand, men det er en mangel på sjoldbruskkjertel- hormoner. Det finnes flere årsaker til at man får denne sykdommen.
Det vi tar opp her er:
Hvordan vitamin B12-mangel er relatert til hypotyreose.
Vitamin B12-mangel forverrer hypotyreose. Noen av symptomene som vi finner ved både B12-mangel og hypotyreose, inkluderer depresjon, sløvhet, tretthet, hukommelsesproblemer og forstyrret søvnmønster.
Skjer det ofte at en person får begge mangler? Dessverre viser det seg at det skjer ganske ofte.
I en studie, som ble publisert i Journal of the Pakistan Medical Association, fant forskerne dette: https://www.ncbi.nlm.nih.gov/pubmed/18655403.
I denne studien undersøkte forskerne tegn på vitamin B12-mangel hos 116 hypotyreosepasienter. Resultatene av studien viste at det var høy forekomst av B12-mangel hos disse pasientene. 39,6 % av pasientene led også av B12-mangel.
KONKLUSJON: Det er en høy (ca. 40%) prevalens av B12-mangel hos hypotyroide pastienter. Screening for vitamin B12- nivåer bør gjennomføres hos alle hypothyroide pasienter, uavhengig av deres skjoldbruskantistoffstatus.
B12-nivåene hos denne pasientgruppen bør ligge nær øvre grense for det akseptable området for B12-nivå hos friske pasienter.
https://stopthethyroidmadness.com/2009/03/18/have-you-tested-your-b12/
B12 - the vitamin that goes low in many thyroid patients
Kliniske studier har vist at B-12 mangelen er like vanlig hos unge og eldre.
En annen studie viser at hypotyreose er årsak til B12-mangel.
Se studien i Annals of Internal Medicine.
Denne studien viser at pasienter med hypotyreose vanligvis har høye homocysteinnivåer.
Det ble konkludert med at pasienter med rett behandling med skjoldbruskkjertelhormoner kunne unngå B12-mangel.
Hvorfor er dette relatert til vitamin B12?
Homocystein er en metabolitt av den viktige aminosyren metionin som krever vitamin B12 og folat til synteseprosessen. De utilstrekkelige nivåene av disse vitaminene fører til akkumulering av homocystein i kroppen.
Som et resultat blir homocystein giftig for kroppens nerve- og kardiovaskulære system. Derfor er det nødvendig med tilskudd med vitamin B12, og eller folat i tilfelle mangel i ett eller begge næringsstoffer, for å forhindre akkumulering av homocystein.
Skjoldbruskhormoner deltar i folatesyntesen, som igjen påvirker disse hormonene samt kobalaminnivåene i blodet.
I utgangspunktet kan hypotyreose føre til vitamin B12-mangel, fordi tilstanden påvirker absorpsjon av mikronæringsstoffer.
Du kan lese mer om hypotyreose og sammenhengen med B12
https://thyroidea.no/fagstoff/vitaminer-mineraler/
10-40% af patienter med Hashimoto's har atrofisk gastritt og er dermed i høyrisiko for at utvikle B12 mangel!
Hashimoto's Thyroiditis and Autoimmune Gastritis
Abstract
The term "thyrogastric syndrome" defines the association between autoimmune thyroid disease and chronic autoimmune gastritis (CAG), and it was first described in the early 1960s. More recently, this association has been included in polyglandular autoimmune syndrome type IIIb, in which autoimmune thyroiditis represents the pivotal disorder. Hashimoto's thyroiditis (HT) is the most frequent autoimmune disease, and it has been reported to be associated with gastric disorders in 10-40% of patients while about 40% of patients with autoimmune gastritis also present HT. Some intriguing similarities have been described about the pathogenic mechanism of these two disorders, involving a complex interaction among genetic, embryological, immunologic, and environmental factors. CAG is characterized by a partial or total disappearance of parietal cells implying the impairment of both hydrochloric acid and intrinsic factor production. The clinical outcome of this gastric damage is the occurrence of a hypochlorhydric-dependent iron-deficient anemia, followed by pernicious anemia concomitant with the progression to a severe gastric atrophy. Malabsorption of levothyroxine may occur as well. We have briefly summarized in this minireview the most recent achievements on this peculiar association of diseases that, in the last years, have been increasingly diagnosed.
Keywords: thyroiditis, polyglandular autoimmune syndrome, thyroxine malabsorption, gastric atrophy, pernicious anemia, Helicobacter pylori infection, cellular immunity.
Les artikkelen: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5405068/?fbclid=IwAR32Esmbo24AhZIHEIhJ5LgbVv382aXrS6XHqN6wJxIKaymiZrfeXEtuvn8
Changes in metabolic and cardiovascular risk factors before and after treatment in overt hypothyroidism.
Kutluturk F1, Yuce S, Tasliyurt T, Yelken BM, Aytan P, Ozturk B, Yılmaz A.
Author information
Abstract
AIM:
Overt hypothyroidism is associated with an increased risk for developing cardiovascular disease. We aimed to assess the changes in renal function, serum lipids, vitamin B12, folic acid and homocysteine levels before and after treatment in hypothyroid patients.
METHODS:
The study included 54 patients (F/M=47/7) with overt hypothyroidism. All patients were assessed for demographic characteristics such as age, gender, body weight, and body mass index. Fasting blood samples were taken from the patients for analysis of chemical parameters including thyroid stimulating hormone (TSH), free thyroxine (fT4), homocysteine, total cholesterol, triglycerides, low-density lipoprotein cholesterol (LDL), high-density lipoprotein cholesterol (HDL), folic acid, and vitamin B12 levels before and after L-thyroxine (LT4) treatment.
RESULTS:
Homocysteine levels in hypothyroidism (9.67 ± 5.24 mmol/l) were significantly higher than in euthyroid state (8.16 ± 3.38 mmol/L, p=0.038). Glomerular filtration rate (GFR) was lower before treatment. Following LT4 replacement, renal functions significantly improved. After achieving the euthyroid state, folic acid levels significantly increased although vitamin B12 levels were not changed. There was a significant reduction in serum lipid levels after LT4 replacement. It was demonstrated that there was a significant negative correlation between GFR and lipids and a positive correlation with homocysteine and lipids at hypothyroid state. After normalization of thyroid functions, the correlations became non-significant.
CONCLUSION:
The hypothyroidism was associated with increased serum homocysteine, lipids, and creatinine concentrations. The improvement of these parameters with LT4 replacement may be associated with the lower risk for atherosclerotic cardiovascular diseases in the patients with hypothyroidism.
https://www.ncbi.nlm.nih.gov/pubmed/23892857?fbclid=IwAR1d7hN5BQiFtrfhzUFbGr2UWugnrKSktGlRf_41yyoVG1kfsjzKMN7PmkI
Vitamin B12 deficiency common in primary hypothyroidism
Abdul Jabbar 1, Aasma Yawar, Sabiha Waseem, Najmul Islam, Naeem Ul Haque, Lubna Zuberi, Ataullah Khan, Jaweed AkhterAffiliations expand- PMID: 18655403
Erratum in
- J Pak Med Assoc. 2009 Feb;59(2):126. Wasim, Sabeha [corrected to Waseem, Sabiha]
Abstract
Objective: To assess the prevalence and clinical features of B12 deficiency in hypothyroid patients and to evaluate clinical response in symptoms to B12 replacement therapy.
Methods: One hundred and sixteen hypothyroid patients from our endocrine clinic were evaluated for signs and symptoms of vitamin B12 deficiency. Laboratory parameters including Haemoglobin (Hb), MCV, Vitamin B12 levels and presence of anti thyroid antibodies were analyzed. Patients with low B12 levels were treated with parenteral intramuscular vitamin B12 monthly, and monitored for improvement of symptoms.
Results: A total of 116 patients (95 females and 21 males) were evaluated. Forty six (39.6%) hypothyroid patients had low vitamin B12 levels. Males and females had the same prevalence of B12 deficiency. Generalized weakness, impaired memory, depression, numbness and decreased reflexes were more frequently noted in B12 deficient patients, but failed to achieve statistical significance when compared with B12 sufficient patients. The mean Hb in B12 deficient group was 11.9 +/- 1.6 mg/dl and 12.4 +/- 1.7 mg/dl in the B12 sufficient group, however the mean MCV did not differ in the two groups. Patients with B12 deficiency did not have a higher prevalence of anaemia. Thyroid antibodies were checked in half the patients and 67% had positive titers for anti thyroid antibodies. Prevalence of vitamin B12 deficiency did not differ in patients with positive antibodies (43.2%) compared to those with negative antibodies (38.9%) (p= 0.759). Twenty four hypothyroid patients with B12 deficiency received intramuscular vitamin B12 injections monthly and improvement in symptoms was noted in 58.3% of these subjects. Additionally, 21 subjects complained of symptoms consistent with B12 deficiency but who had normal range B12, levels and were prescribed monthly B12 injections and 8 (40%) had good subjective clinical response at 6 months.
Conclusions: There is a high (approx 40%) prevalence of B12 deficiency in hypothyroid patients. Traditional symptoms are not a good guide to determining presence of B12 deficiency. Screening for vitamin B12 levels should be undertaken in all hypothyroid patients, irrespective of their thyroid antibody status. Replacement of B12 leads to improvement in symptoms, although a placebo effect cannot be excluded, as a number of patients without B12 deficiency also appeared to respond to B12, administration.
https://pubmed.ncbi.nlm.nih.gov/18655403/
Framingham Offspring-studien (Tucker et al., 2000, Am J Clin Nutr 71:514–22)
Bakgrunn
Vitamin B12-mangel forbindes både med megaloblastanemi og nevrologiske symptomer som sensorisk tap, ataksi, parestesier og kognitive/messige endringer. Tidligere ble "lav-normal"-nivåer ofte vurdert som ufarlige, men studier viste at nevrologiske symptomer kunne oppstå også ved verdier innenfor dette området. Samtidig ble det uttrykt bekymring for at folsyretilskudd kunne maskere hematologiske tegn på B12-mangel, men ikke hindre nevrologiske skader.
Hos eldre er tap av magesyre og atrofisk gastritt velkjente risikofaktorer, men hvor stor del av B12-mangelen som kan forklares av slike mekanismer var uklart.
Formål
Studien undersøkte:
Hvor utbredt lavt plasma-B12 er i en stor befolkningsgruppe (2999 voksne, 26–83 år).
Om B12-nivåer varierer med inntakskilder (kjøtt, meieriprodukter, frokostblanding, kosttilskudd).
Metode
Data fra Framingham Offspring Cohort, 5. undersøkelsesrunde (1991–1995).
2999 deltakere med blodprøver og valide kostholdsdata.
Plasma B12 målt med radioassay.
Kosthold kartlagt med et 126-punkts spørreskjema.
Cutoff brukt: <148 pmol/L (tradisjonelt "mangel"), <185 pmol/L (bedre samsvar med forhøyet MMA), <258 pmol/L (mulig klinisk betydning).
Hovedfunn
Prevalens
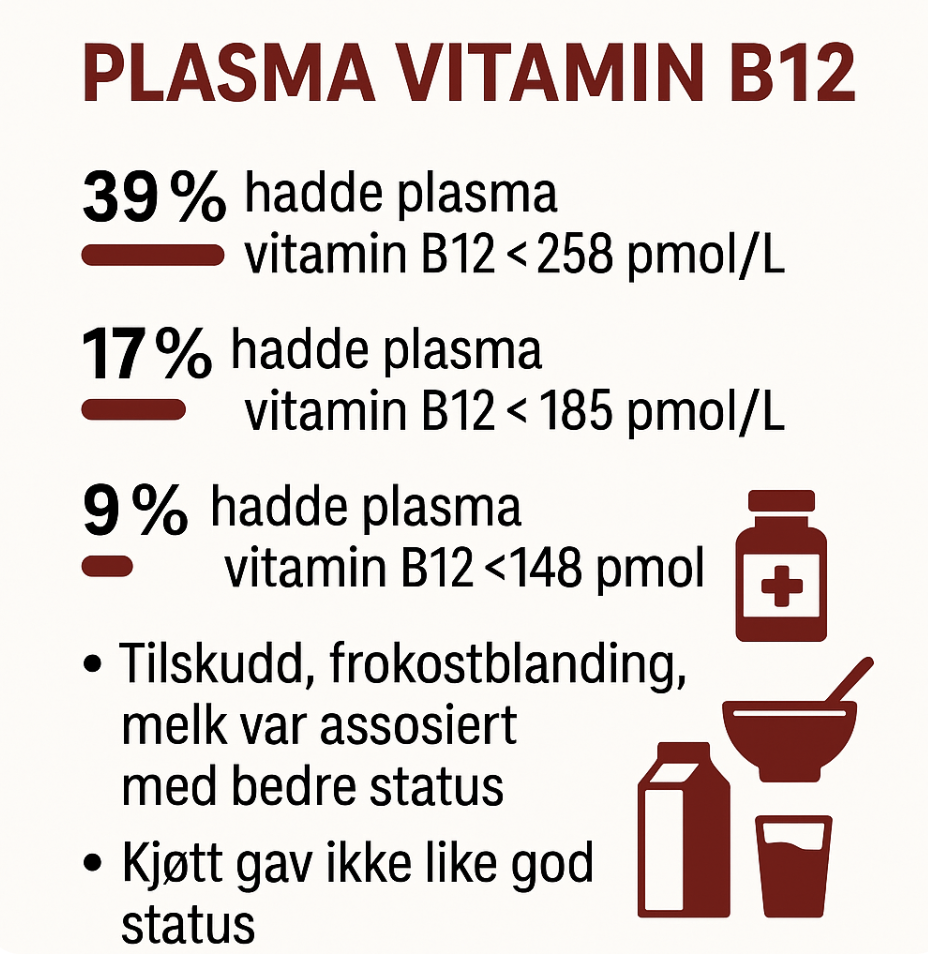
39 % hadde B12 <258 pmol/L.
17 % hadde B12 <185 pmol/L.
9 % hadde B12 <148 pmol/L.
Ingen store forskjeller mellom aldersgruppene (26–49, 50–64, 65–83 år).
Kosttilskudd
Brukere av tilskudd hadde klart bedre status.
Kun 8 % av tilskuddsbrukere hadde <185 pmol/L, mot 20 % blant ikke-brukere.
Frokostblanding
Ikke-brukere av tilskudd som spiste beriket frokostblanding >4 ganger/uke hadde lavere risiko for lave nivåer (12 % <185 pmol/L) enn de som aldri spiste frokostblanding (23 % <185 pmol/L).
Meieriprodukter vs. kjøtt
Meieriinntak var sterkt knyttet til bedre B12-status: høyeste tertil hadde kun 13 % <185 pmol/L mot 25 % i laveste tertil.
For kjøtt var sammenhengen svakere – selv om kjøtt bidro med mest B12 totalt, var det ikke like effektivt for å opprettholde høye plasmanivåer.
Statistisk analyse viste at B12 fra meieri og frokostblanding var betydelig mer biotilgjengelig enn fra kjøtt.
Clusteranalyse
Seks ulike inntaksmønstre ble identifisert.
"Kjøtt-gruppen" hadde lavere plasma-B12 enn de som fikk mye fra melk eller frokostblanding, selv ved samme totale inntak.
Odds ratio for å ha <185 pmol/L var høyest i kjøtt-gruppen (2,4 sammenlignet med supplement-brukere).
Diskusjon
Studien dokumenterte en uventet høy forekomst av lavt plasma-B12 også hos yngre voksne, ikke bare eldre.
Dette kan ha klinisk betydning fordi symptomer kan oppstå selv ved "lav-normal" status.
Viktig implikasjon: inntakskilde betyr mer enn bare mengde.
B12 i kosttilskudd, berikede kornprodukter og melk ser ut til å være mer biotilgjengelig enn B12 fra kjøtt.
Mulige forklaringer: varmebehandling av kjøtt kan ødelegge B12, mens B12 i melk og berikede matvarer foreligger i en friere form som absorberes bedre.
Konklusjon
Nesten 40 % av deltakerne hadde plasma-B12 under 258 pmol/L, en konsentrasjon assosiert med risiko for symptomer og forhøyet homocystein.
Kosttilskudd og berikede matvarer hadde en klar beskyttende effekt.
Meieriprodukter var bedre assosiert med høyere B12-status enn kjøtt.
Resultatene støtter anbefalingen om at særlig personer over 50 år bør sikre seg B12 gjennom tilskudd eller berikede matvarer, men peker også på at yngre voksne kan være utsatt.

